Approximately 25% of diabetics will develop a foot wound or ulcer in their lifetime. Amputation in people with diabetes is 10 to 20 times more common than in people without diabetes6. Every year, more than one million of leg amputations are performed globally because of diabetes, which is equivalent to one leg amputation every 30 seconds7.
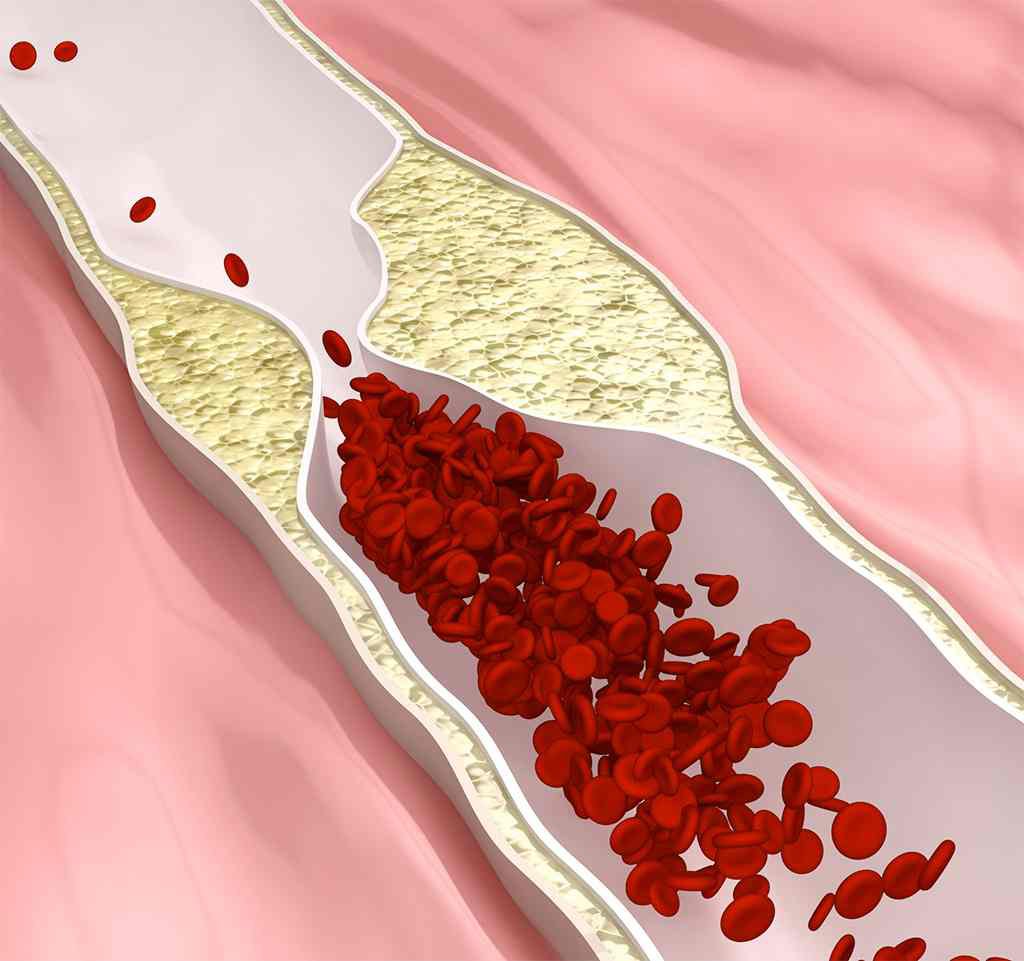
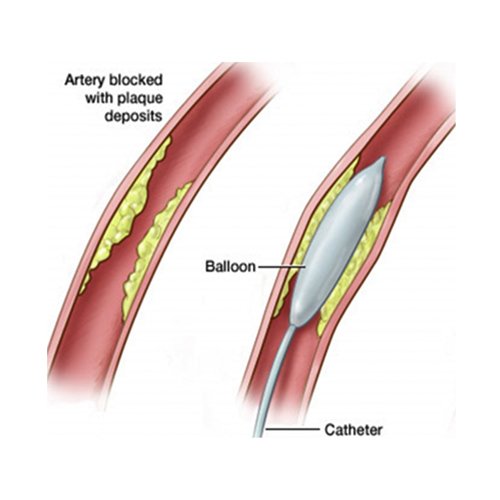
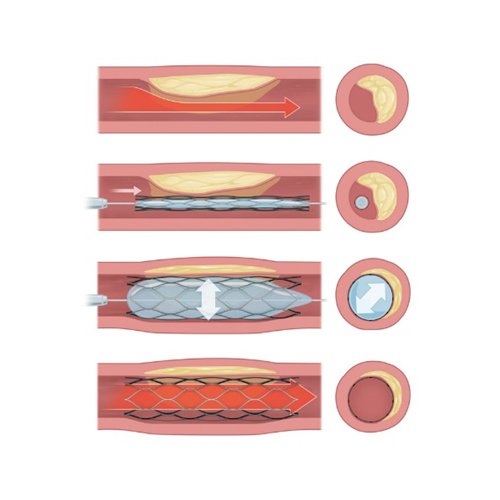
In a person with diabetes, higher than normal sugar levels in the body will over time damage nerves (neuropathy)8 and cause blood vessels of the leg and foot to narrow and harden (atherosclerosis) leading to reduced blood flow down to the feet (Peripheral Arterial Disease (PAD))9.
a) Diabetic neuropathy8- This can result in:
- Poor sensation in the feet- Minor injuries to the foot can be left undetected because of poor sensation and may consequently lead to foot ulceration and infection.
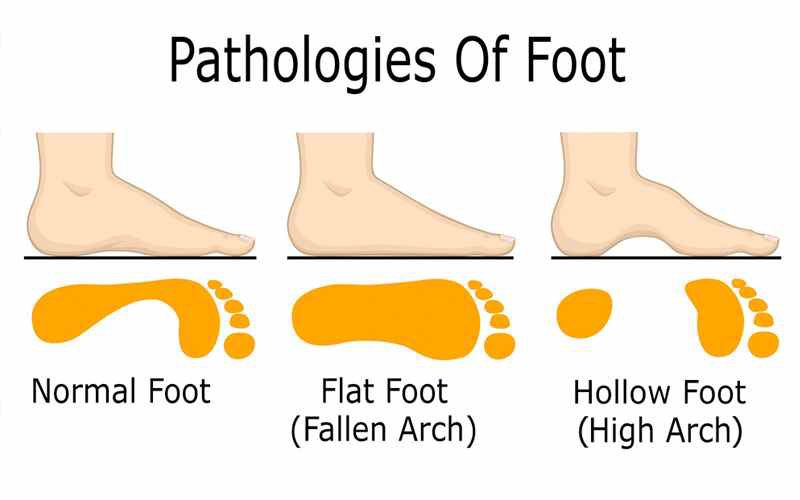
- Foot deformities- Structural changes in the foot such as hammer toes, claw toes, collapse of the midfoot (Charcot foot) and limited joint mobility can result in focal areas of high pressure on the sole. Skin can break down over pressure points leading to ulceration.
- Decreased sweating- Nerves supplying the sweat glands stop functioning, leading to dry, flaky and cracked skin. Cracked skin in the foot may allow bacteria to enter and cause infection.
b) Peripheral Arterial Disease (PAD)9 – People with diabetes are at increased risk of atherosclerosis which narrows and harden the blood vessels of the leg and within the foot. Poor blood supply to the foot will lead to poor healing and gangrene as well as reduced ability to fight infection.