What is Glaucoma?

Normal Visual Field
Glaucomatous Visual Field Defect
Glaucoma is a disease of the optic nerve (an optic neuropathy), the nerve which connects the eyeball to the brain. A normal functioning nerve is essential for good vision and conversely a nerve which is not functioning well, as in glaucoma, will often negatively influence visual function. Specifically, in glaucoma, the type of visual dysfunction is in the peripheral visual field. The central vison, what people read on the vision charts, if often normal, even in advanced glaucoma. This helps explain why glaucoma has been assigned the moniker "the thief of sight" – because people with glaucoma may not be aware they have the disease because their central vision remains normal. In other words, the disease is essentially asymptomatic.
Normal Visual Field
Glaucomatous Visual Field Defect
Thankfully, blindness as a result of glaucoma is rare, especially in developed countries. Worldwide there are thought to be over 70 million people with glaucoma and approximately 10% of those will be blind1. The definition of blindness, according to the World Health Organisation, is visual acuity of 3/60 or worse (or a severely constricted visual field) in a patient's better eye. This makes glaucoma the leading cause of irreversible blindness worldwide (as opposed to reversible blindness due to cataract or refractive error for example).
Types of Glaucoma
There are several types of glaucoma but broadly they can be divided in to 4 groups.
The first division is in to primary and secondary, i.e. depending if the glaucoma is independent of any other concurrent eye disease (primary) or consequent to concurrent eye disease (secondary). Some examples in the latter group include glaucoma secondary to trauma, glaucoma secondary to diabetes induced neovascularisation of the anterior segment and glaucoma secondary to uveitis.
The second division is in reference to the drainage angle which is located in the anterior segment of the eye. Specifically, it refers to the area responsible for egress of fluid from the eye's anterior chamber – if this area is not working properly, the outflow of fluid will be restricted and the eye pressure, or intraocular pressure (IOP), will increase. If the drainage angle is blocked by the peripheral iris, the angle is referred to as 'closed'. If the angle is not obstructed but dysfunctional, it is referred to as 'open'.
Based on these classifications, glaucoma can be divided into 4 basic groups: primary open-angle glaucoma (POAG), primary angle-closure glaucoma (PACG), secondary open-angle glaucoma and secondary angle closure glaucoma. By far, POAG and PACG are the most common types, with POAG more prevalent than PACG.
PACG is a particular problem in East Asia (including Singapore) as this type of glaucoma is more common in people of East Asian origin than in Caucasians, Africans or South Asians. One condition which can lead to PACG is Acute Angle-Closure (ACC). This condition, one of the few true ophthalmic emergencies, presents with the onset (usually over a period of a few hours) of severe pain, blurred vision and red eye. These symptoms are due to very high IOP which needs to be lowered quickly to reduce the symptoms and decrease the risk of permanent damage to the eye. PACG also results in more blindness proportionally than POAG, which is why glaucoma blindness in Asia is a particular problem
Diagnosis and treatment
The aim of glaucoma treatment is to improve/maintain quality of life - which broadly means reducing the risk of visual loss. As mentioned earlier, glaucoma is a disease of the optic nerve yet none our current treatment strategies specifically target the optic nerve. Despite much research on this topic, no one has yet developed any treatment that is directly targeted to the optic nerve. Instead, all our treatments are directed towards the lowering of IOP. This is because are now several major landmark studies which prove that lowering of IOP both lowers the risk of developing glaucoma (in certain situations) and reduces the risk of worsening of glaucoma2-5.
The relationship between IOP and glaucoma is a complicated one and beyond the scope of this short review. Suffice to say, although there is an association between high IOP and an increase the likelihood of developing glaucoma, the relationship is not a straightforward one. There are many people with raised IOP who never develop glaucoma and there are many people with normal IOP who do develop glaucoma. In terms of patients with established glaucoma, lowering the IOP to a certain level (approximately 20-50% reduction from the baseline IOP) is beneficial in slowing down the disease deterioration, although the management needs to be balanced with the effect of treatment on the patient's quality of life.6
There are several ways in which IOP can be lowered. Topical medications (i.e. eye drops) are often given as first-line and there are several different types available. Laser treatment is also possible in some instances, for example selective laser trabeculoplasty (SLT) or trans-scleral cyclophotocoagulation (TCP). Surgical treatment, for example 'trabeculectomy' or insertion of a glaucoma drainage device (GDD or 'tube') are usually reserved for more serious disease or disease which is deteriorating despite medications and/or laser. Such surgery is not without risk of course and the decision to perform surgery is not straightforward.
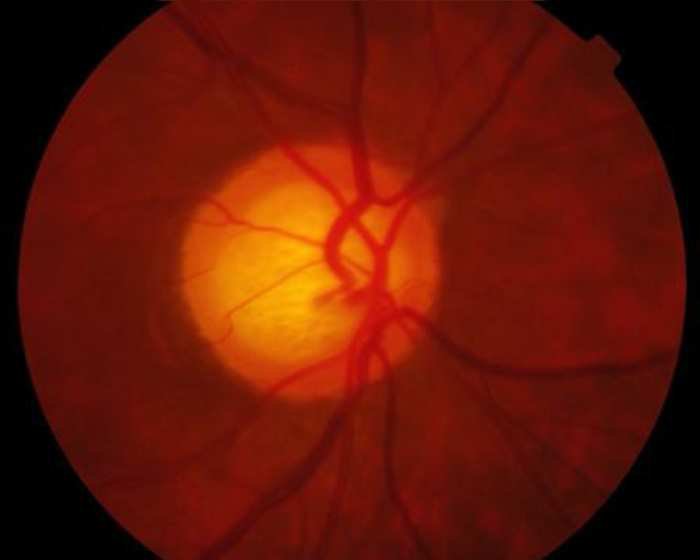
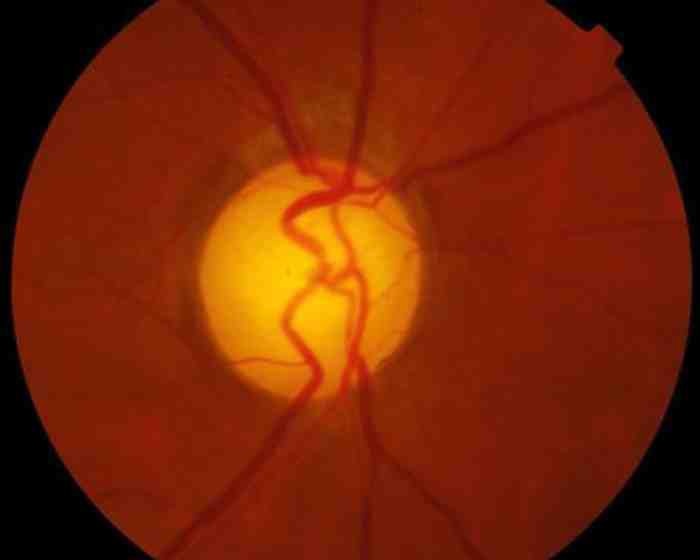
Diagnosing and monitoring glaucoma involves examination of the optic disc and investigations such as visual field testing (a form of functional testing) and/or optical coherence tomography (OCT), a form of structural testing. These tests are typically performed by specialist technicians and the results reviewed by the specialist ophthalmologist who will then make a management decision.
Glaucoma management during pandemic
An interesting development in the field of glaucoma management, is the recent interest and implementation of 'virtual clinics'. This came about after a realisation that a proportion of glaucoma patients (typically those with mild and/or stable disease) could be managed appropriately as long as the specialist is able to review the patient's data such as IOP, visual acuity and investigations. This has meant that as long as the patient has these data collected (which could be done outside of the main hospital setting), the patient need not see the doctor "face-to-face" as is the current protocol.
The benefits of this system are multiple and in regards the COVID-19 pandemic, have become essential. As we move towards a post COVID-19 world it is likely that these models of care will continue as they have been shown to be safe, cost-effective and popular amongst patients and healthcare staff alike. A subset of virtual clinic, video consultation, is also gaining popularity as the world has become accustomed to video platforms such as Zoom.
Conclusion
In summary, glaucoma is a serious disease which can result in irreversible blindness but thankfully this are treatment modalities are aimed at improving or maintaining quality of life and involve lowering IOP. Mild or stable glaucoma can be managed safely with virtual clinics and this is an exciting and developing area in glaucoma at this time.
By Dr Rahat Husain
Senior Consultant Ophthalmologist, Glaucoma Service, Singapore National Eye Centre
Director, Regional/Community Eyecare (SingHealth)
Adjunct Associate Professor, Duke-NUS Graduate Medical School
Adjunct Senior Clinician Investigator, Singapore Eye Research Institute
Senior Consultant Ophthalmologist, Glaucoma Service, Singapore National Eye Centre
Director, Regional/Community Eyecare (SingHealth)
Adjunct Associate Professor, Duke-NUS Graduate Medical School
Adjunct Senior Clinician Investigator, Singapore Eye Research Institute
This article was contributed by A/Prof Rahat Husain, AIA Preferred Provider, and Senior Consultant Ophthalmologist of Singapore National Eye Centre. To request an appointment with Dr Husain, please click here.
References
- Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262-267.
- Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701-713.
- Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M; Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression. Arch Ophthalmol. 2002;120(10):1268-1279.
- The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS), 7: the relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130(4):429-440.
- Lichter PR, Musch DC, Gillespie BW, et al; CIGTS Study Group. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108(11):1943-1953.
- American Academy of Ophthalmology Preferred Practice Patterns Committee GP. Preferred practice pattern: primary open-angle glaucoma. In: Ophthalmology. Chicago, Illinois: American Academy of Ophthalmology: 2010.


